What is this rampant infection? one may question. Is it a staph infection? A “superbug” such as MRSA? Pneumonia?
In reality, the dreaded illness is the seemingly humble urinary tract infection. It affects hundreds of thousands of patients annually in our healthcare system. It is easy to dismiss a urinary tract infection with simple antibiotics or a regimen of cranberry juice, but it can lead to a host of secondary infections and illnesses. UTIs affect every part of the urinary system, including the lower urinary tract (manifesting itself as a bladder infection), upper urinary tract (resulting in the more painful kidney infection), urethra, and ureters. Furthermore, a typical UTI may quickly develop into periurethral abscess, epididymitis, cystitis, or the serious and often fatal urosepsis or bacteremia, infections of the bloodstream.
Urinary tract infections in a professional healthcare setting
Catheterization – a process in which a thin tube is inserted into a patient’s bladder via the urethra to drain urine – in a hospital, rehabilitation center, or nursing facility is frequently necessary due to incontinence or debilitation due to surgical procedures, illness, or injury. Approximately 15-25% or all hospitalized patients will require a catheter; however, roughly 75% of nosocomial (hospital-acquired) UTIs are associated with catheterization[4]. The increased risk of developing a catheter-associated urinary tract infection (CAUTI) with prolonged catheterization is well documented.
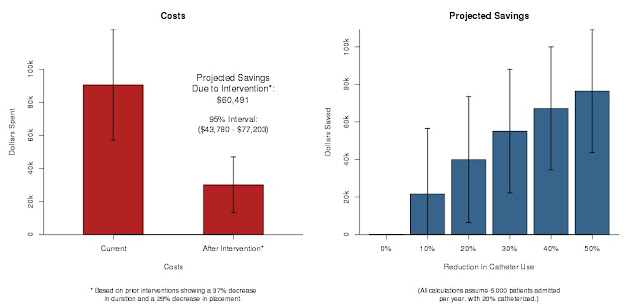
Costs increase dramatically with CAUTI; since October of 2008, Medicare and Medicaid no longer pay for care associated with CAUTI[5]. Assuming a facility admits 3,000 adult patients yearly and 20% of those require a catheter, the facility may expect to save approximately $36,295 annually with proper intervention (reducing duration by an average of 37% and catheter placement by 29%) and preventative measures against unnecessary catheterization and CAUTIs[6].
Incontinence and UTIs in home care
Recent statistics show that incontinence is widespread among the population over the age of fifty, hovering at about fifty percent. The older one gets, the greater the chance of developing incontinence. As the baby boomer population ages, the prevalence of incontinence is expected to rise. When patients with incontinence are bedridden or mobility impaired, catheterization is often recommended. Home catheterization carries the same risks as institutional catheterization, but with increased risk of infection due to factors such as less vigilant or skilled care, reduced standards of hygiene, and exposure to various bacteria. The risk of UTI in home care settings is estimated to be 6.5 times higher in catheterized patients than non-catheterized patients[7].
How can CAUTI be prevented?
Thanks to advances in medical equipment, catheterization can be performed differently for better results or even avoided entirely. Specialized catheters reduce the possibility of CAUTI, and manufacturers such as Medline produce and promote innovative solutions to CAUTI risk. Revolutionary bladder scanners help patients with incontinence, surgical ramifications, or various illnesses relearn the sensation of needing to urinate, resulting in reduced time or complete elimination of catheterization.
Medline ERASE CAUTI system
Industry-leading manufacturer Medline offers the ERASE CAUTI program to hospitals, skilled nursing facilities, and other healthcare providers. The program utilizes a catheter management system that encourages staff in the proper usage of catheters and related supplies. Using the simple acronym ERASE, the system reminds staff of every step necessary to prevent urinary tract infections in patients using catheters: Evaluate indications, Read directions, Aseptic technique, Secure catheter, and Educate the patient. Following this routine has been proven to reduce CAUTI rates by an average of 70% and catheterization rates by 16%.
 |
| Silvertouch Foley Catheter Tray |
The system’s effectiveness is due to its educational foundation as well as innovative catheters and trays to prevent CAUTI in patients who truly need catheterization. The Silvertouch® 100% silicone Foley catheter incorporates a silver hydrophilic coating with a patented process that covalently binds silver ions to the lubricious latex-free finish. Silver ions are renowned for their antimicrobial properties; with the combination of the absorbent coating and silver ions, the catheter is designed to remain safely and comfortably in place for seven days while fighting bacteria and fungi.
 |
| Silvertouch Foley Catheter |
Bladder scanner
 |
| BioCon®-500 Bladder Scanner |
The device also allows users to monitor the patient's bladder volume and voided amounts. Clinicians may observe consistent patterns in bladder volume and adjust fluid intake as necessary. The scanners feature specialized child, male and female modes for the most accurate readings. A portable unit is brought to the resident's bedside and the patient prepared with clear conductive gel. The wand is then positioned over the bladder area, where it "reads" bladder information and transmits it to the screen. In less than five minutes, the device calculates the bladder volume and displays an image of the bladder.
 |
| BioCon® CubeScan 700 Bladder Scanner |
The bladder scanners feature a variety of advanced capabilities such as a pre-scan feature to ensure proper placement, high-capacity memory, PC and EMR compatibility, integrated printing, and/or voice recording. They provide patients with non-invasive, comfortable screening and dignity preservation during times that can be wrought with humiliating procedures. Their straightforward operation makes them accessible to virtually anyone and requires little training, promoting staff efficiency while effectively reducing the rate of unnecessary catheterization and painful CAUTI.
What does my facility or caretaker need to prevent CAUTI?
Being that CAUTI is the most prevalent infection in healthcare today, virtually anyone is at risk of contracting it. Proper education and appropriate supplies have been proven to drastically reduce CAUTI rates in both home and healthcare settings. At Tiger Medical Supplies, we are dedicated to providing you with the tools you need to keep yourself or your patients comfortable, healthy, and financially secure. Contact one of our capable customer service representatives or visit our website to join the anti-CAUTI initiative today.
[7] Getliffe, Kathryn and Newton, Teresa; Catheter-associated urinary tract infection in primary and community health care


No comments:
Post a Comment